Department of Radiation Oncology
01What we do
Director
Satoshi Itasaka
The Department of Radiation Oncology has resulted from the division of the radiology department into a radiation oncology and diagnostic radiology department. Our team is made up of radiologists, therapeutic medical physicists, radiation quality managers, radiotherapy nurses and administration staff, and we take care of over 700 cases annually.
Radiotherapy began in this hospital in 1992, when the hospital obtained linear accelerator, intracavity irradiation and radiation therapy (simulation) facilities. Since then, we have commenced other precision therapies, including external beam radiation, whole body irradiation, and cranial stereotactic radiotherapy. We became part of the Japanese Society for Radiation Oncology in 2004, and we work with other departments within the hospital in a multi-disciplinary approach for the best care outcomes for the patient.
02Therapies undertaken in this department
1. Image-guided radiotherapy (IGRT)
We have been undertaking this therapy since 2010. It involves using x-ray and cone-beam computed tomography (CT) to take an image of the diagnosed area, which is then compared to a normal image of the same area to allow for precise correcting and adjustment of the targeted therapy area.
2. Intensity-modulated radiation therapy (IMRT)
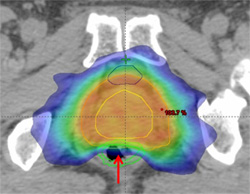 Image 1: IMRT image showing radiation distribution in the prostate gland. The arrow shows the reduction of radiation in the anterior and posterior of the rectum.
Image 1: IMRT image showing radiation distribution in the prostate gland. The arrow shows the reduction of radiation in the anterior and posterior of the rectum.
This therapy delivers a single radiation beam while changing the intensity in different areas of the beam, which maximizes the concentration of the radiation to the targeted legion, and thus minimizes damage to the surrounding normal tissues. We commenced IMRT therapy in 2005, with this therapy requiring an experienced operator. The main cancers targeted with this therapy include those of the prostate, the cranial area, and the neck. In 2011, we began using volumetric-modulated arc therapy (VMAT), which delivers the same therapy in a shorter time.
3. Stereotactic radiotherapy
We commenced this therapy in 1995, and it involves targeting the tumor with a concentrated dose of radiation using a three-dimensional computerized model taken before the therapy. We now use the micro-multi-leaf collimator, which enables us to undertake this therapy for all types of tumors with a higher accuracy.
We commenced stereotactic body radiation therapy in 2005, which we mainly use for small tumors of the lung and tumors of the spine. This therapy can accurately target radiation within an area of a few millimeters, and we are getting the same favorable results for early-stage lung cancer as surgery, with minimal side-effects.
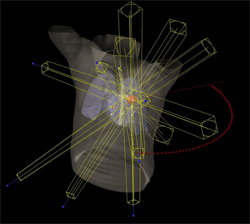 Image 2: Image showing beam distribution of stereotactic radiotherapy in a case of lung cancer.
Image 2: Image showing beam distribution of stereotactic radiotherapy in a case of lung cancer.
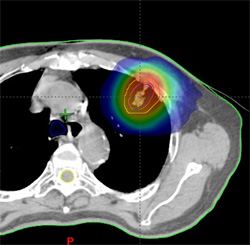 Radiation distribution image of the same case.
Radiation distribution image of the same case.